What is Donor Conception via IVF with Donor Gametes?
Donor conception, at its core, refers to the creation of a family using reproductive cells (gametes) donated by someone outside the intended parenting unit.

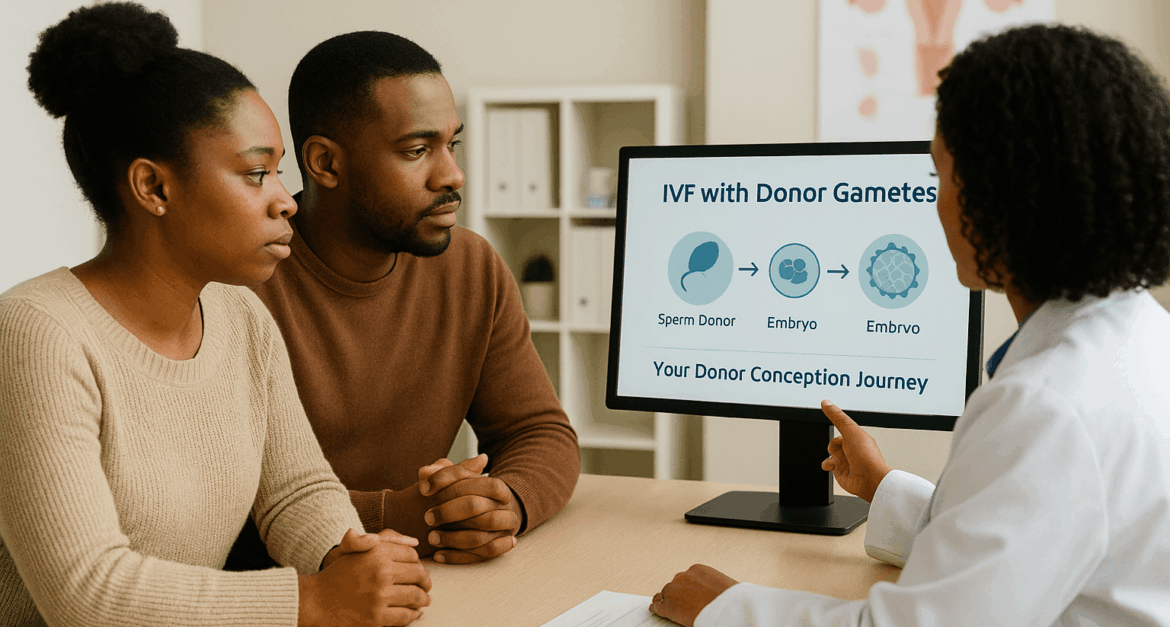
When this process occurs through In Vitro Fertilization (IVF), it involves a series of precise laboratory and medical procedures. Unlike traditional IVF, where a couple uses their own eggs and sperm, donor conception means that at least one, or sometimes both, of the gametes come from a third-party donor.
This fundamental difference means the child will not share genetic material with the parent who did not contribute their own gamete, or with either parent if donor embryos are used.
The general steps for donor conception via IVF follow a structured fertility treatment pathway. It begins with a thorough consultation and assessment of the intended parent(s) to determine suitability and discuss options.
Next is donor selection, where individuals or couples choose an egg donor, sperm donor, or embryo donor from a reputable source. Once a donor is chosen, the process moves to gamete retrieval or thawing (if frozen gametes are used).
The donor eggs are then fertilized with sperm in a laboratory dish—this is the “in vitro” part of IVF. The resulting embryos are carefully monitored as they develop. Finally, the healthiest embryo is selected for embryo transfer into the recipient’s uterus. A pregnancy test and follow-up confirm the outcome and provide ongoing care. This entire sequence is a carefully managed journey toward donor conception.
Who Benefits from Donor Conception?
Donor conception offers a viable and often highly successful path to parenthood for a wide range of individuals and couples. One common scenario involves advanced maternal age or a diagnosis of diminished ovarian reserve, where a woman’s own egg quality or quantity is insufficient for a successful pregnancy.

Similarly, couples who have experienced recurrent IVF failures with their own gametes may find renewed hope with donor eggs.
For those facing male factor infertility, donor sperm IVF becomes the primary solution, allowing them to build a family. Another significant reason for pursuing donor conception is the risk of passing on genetic conditions.
Using donor gametes can prevent the inheritance of specific hereditary diseases. Beyond medical necessity, donor conception is also a transformative option for same-sex couples seeking donor conception and single parents by choice who wish to experience pregnancy and childbirth.
Furthermore, individuals with certain medical conditions affecting gamete production due to illness or treatment can also achieve their dream of parenthood through this pathway. Donor conception truly broadens the horizons of family building.
The Donor Selection Process: Finding Your Match for Donor Conception
One of the most significant decisions in your journey toward donor conception is whether to choose an anonymous donor or a known donor. Each option carries distinct advantages and considerations. Anonymous donation, typically facilitated through reputable sperm banks or egg donor agencies, offers a level of privacy and often a wider selection of available donors.
For many, this anonymity provides a sense of emotional distance, allowing them to focus solely on their role as parents without the complexities of a direct relationship with the donor.
However, it is important to recognize that even “anonymous” donation may involve the possibility of future contact, depending on the laws of the jurisdiction and the donor’s willingness to be identified to the donor-conceived child upon maturity.
Conversely, choosing a known donor—often a family member or close friend—creates a direct genetic link and can foster a deeper sense of connection and transparency within the family from the outset. This path allows for open communication about the child’s origins and can provide the child with access to their genetic history and potentially a relationship with the donor.
While this can be incredibly enriching, it also introduces complex interpersonal dynamics that require careful navigation. It is absolutely crucial to seek legal counseling for known donations in donor conception.
This step ensures that all parties understand their rights, responsibilities, and the legal implications regarding parental status, financial obligations, and future contact, minimizing potential disputes down the line. The decision between anonymous and known donation is deeply personal, influenced by individual values, comfort levels, and long-term family goals for donor conception.
The Rigorous Screening Process for Donor Conception Candidates
Regardless of whether you choose an anonymous or known donor, a rigorous screening process is a non-negotiable step in ensuring the safety and success of donor conception. This comprehensive evaluation is designed to protect both the intended parents and the future child.
For both egg and sperm donors, this involves extensive medical screening to rule out infectious diseases and assess overall health. Donors undergo thorough physical examinations, blood tests, and urine tests.
Beyond medical health, genetic screening is paramount. Donors are tested for a wide range of inherited conditions, including cystic fibrosis, spinal muscular atrophy, and chromosomal abnormalities, to minimize the risk of passing on genetic diseases to the donor-conceived child.
A detailed family medical history is also compiled to identify any potential predispositions. Finally, psychological screening is a critical component.
Mental health professionals assess the donor’s motivations, emotional stability, and understanding of the long-term implications of their donation. This ensures they are psychologically prepared for the process and for the reality that a child may be born from their donation. This multi-faceted screening is crucial for safety and successful donor conception outcomes, providing peace of mind to intended parents.
Factors to Consider in Donor Matching for Donor Conception
Finding the right match is a deeply personal aspect of the donor conception journey. While medical suitability is paramount, many intended parents also consider various other factors to find a donor with whom they feel a strong connection.
Clinics and sperm/egg banks often provide detailed profiles that go beyond basic medical information. These profiles may include physical characteristics such as height, weight, hair color, and eye color, allowing intended parents to find a donor who shares certain traits with themselves or their family.
Beyond appearance, many look into the donor’s educational background, interests, and personality. Extended profiles might offer insights into hobbies, talents, and even personal essays or audio recordings, providing a more holistic picture of the individual contributing to donor conception.
While a genetic connection to the donor is established, the influence of environment and upbringing on a child’s personality is also significant. Genetic matching is another key consideration, particularly if one of the intended parents has a known genetic carrier status; cross-referencing donor genetics can further minimize disease risk in the donor-conceived child.
Ultimately, the choice involves a blend of practical considerations and emotional resonance. Ethical and personal considerations play a large role.
Some families prioritize certain values or life experiences in their donor, while others may focus on the donor’s willingness to be contacted in the future. The process of donor selection is a thoughtful, often emotional, step in the journey of donor conception, aiming to find a donor who feels right for your family’s unique story.
Preparing for Your Donor Conception Journey: Recipient Readiness
Once a donor has been selected, the focus shifts to preparing the recipient’s body for pregnancy, a crucial phase in the donor conception journey.
This preparation ensures the uterus is optimally receptive for embryo implantation. The initial steps involve thorough medical evaluations and tests for the recipient.
These typically include blood work to assess hormone levels, infectious disease screening, and a uterine assessment, often through ultrasounds or a hysteroscopy, to identify any structural issues that might impede implantation. The goal is to create the most favorable environment possible for a successful donor conception.
Following these assessments, the recipient will begin a regimen of hormonal medication to prepare the uterine lining. This usually involves estrogen, which helps to thicken the endometrial lining, followed by progesterone, which makes the lining receptive to an embryo.
The timing of these medications is carefully synchronized with the donor’s cycle (if fresh eggs are used) or the embryo’s developmental stage (if frozen embryos are used) to maximize the chances of successful implantation. Beyond medication, lifestyle recommendations are also provided.
These often include advice on maintaining a healthy diet, ensuring adequate rest, and strategies for stress management, all of which contribute positively to the overall health of the recipient and can enhance the prospects of a successful donor conception. Adhering to these guidelines is vital for preparing the body for the significant changes of pregnancy.
The Donor’s Cycle and Gamete Retrieval/Thawing for Donor Conception
The donor’s role in the IVF cycle is distinct, focusing on providing healthy gametes for donor conception. For egg donors, this involves a controlled ovarian stimulation protocol.
The donor receives fertility medications to encourage her ovaries to produce multiple mature eggs in a single cycle. This process is closely monitored through regular ultrasounds and blood tests to track follicle development. Once the eggs are deemed mature, a “trigger shot” is administered, followed by the egg retrieval procedure.
This is a minimally invasive outpatient procedure performed under sedation, where a fertility specialist uses an ultrasound-guided needle to collect the eggs from the donor’s ovaries. These retrieved eggs are then immediately taken to the laboratory for fertilization.
If sperm donors are involved, the process is simpler. A sperm sample is collected, either fresh on the day of egg retrieval or thawed from a previously frozen sample obtained from a sperm bank. For donor embryos, which are already fertilized eggs, the “retrieval” step is replaced by the thawing of the frozen embryos.
The choice between fresh and frozen donor gametes or embryos depends on various factors, including donor availability, logistical considerations, and clinic protocols. Both fresh and frozen options offer excellent success rates for donor conception, providing flexibility in family planning.
Fertilization, Embryo Development, and Transfer in Donor Conception
The laboratory phase is where the magic of donor conception truly begins. Once the donor eggs and sperm are ready, in vitro fertilization (IVF) takes place.
In a traditional IVF setup, the eggs and sperm are placed together in a culture dish, allowing fertilization to occur naturally.
In cases of male factor infertility or if a higher fertilization rate is desired, Intracytoplasmic Sperm Injection (ICSI) may be performed, where a single, healthy sperm is directly injected into each egg. This precise technique significantly enhances the chances of fertilization for donor conception.
After fertilization, the resulting embryos are carefully monitored in the laboratory for several days as they develop. Embryologists assess their growth and quality, looking for optimal cell division and morphology.
This embryo monitoring and selection process is critical for identifying the embryos with the highest potential for successful implantation and a healthy pregnancy. Typically, embryos are cultured to the blastocyst stage (around day 5 or 6 of development) before transfer.
The final step in the medical procedure is the embryo transfer. This is a relatively quick and painless outpatient procedure where the selected embryo(s) are gently placed into the recipient’s uterus using a thin, flexible catheter, guided by ultrasound.
The goal is for the embryo to implant into the uterine lining, marking the beginning of pregnancy and the culmination of the initial stages of donor conception.
The Two-Week Wait and Pregnancy Confirmation in Donor Conception
Following the embryo transfer, intended parents enter what is commonly known as the “two-week wait.” This period, though medically inactive, is often one of the most emotionally challenging phases of the donor conception journey.
It’s a time filled with anticipation, hope, and often anxiety, as the recipient waits to discover if the embryo has successfully implanted and if pregnancy has occurred. Managing expectations during this time is crucial, and many find solace in engaging in light activities, practicing mindfulness, and leaning on their support systems.
At the end of this waiting period, a pregnancy test is performed, typically a blood test that measures the level of human chorionic gonadotropin (hCG), the pregnancy hormone.
A positive result brings immense joy and relief, confirming the successful initiation of pregnancy through donor conception. If the test is positive, subsequent steps involve continued monitoring of hCG levels and early ultrasounds to confirm the viability and location of the pregnancy.
This marks a significant milestone in the donor conception process, transitioning from fertility treatment to prenatal care. Should the test be negative, the clinic will provide guidance on next steps, which may include discussing another cycle or exploring alternative options, always with continued emotional support.
Embracing the Realness: Emotional and Psychological Aspects of Donor Conception
The journey to parenthood through donor conception is rich with emotion, often encompassing a complex interplay of feelings.
For many intended parents, particularly those who initially hoped for a genetically related child, there can be a period of grief for the loss of a genetic connection. This is a valid and natural response, mourning the biological link that won’t exist.
It’s important to acknowledge and process these feelings rather than suppress them. Alongside this, there is immense hope for the future family and the child to come. This emotional journey is rarely linear; it can involve moments of profound joy, anxiety about the unknown, and eventually, a deep sense of acceptance and excitement for the unique path chosen.
Navigating these emotions requires self-compassion and understanding. It’s common to experience a range of feelings, from excitement about the prospect of a baby to moments of doubt or sadness about the circumstances that led to donor conception.
Recognizing that these feelings can coexist is a crucial step. The focus gradually shifts from the method of conception to the reality of impending parenthood, fostering a powerful bond that transcends genetic origins.
Many find that the love and nurturing they offer become the defining factors of their family, making the journey of donor conception a testament to their resilience and commitment.
Open Communication and Support Systems for Donor Conception
One of the most powerful tools in embracing donor conception is open communication. Discussing the donor conception process with your partner, if applicable, is paramount.
This ensures both individuals are on the same page, sharing fears, hopes, and expectations. Extending these conversations to trusted family members and close friends can create a vital network of understanding and support. Choosing whom to share this information with is a personal decision, but having a supportive community can significantly ease the emotional load.
Beyond personal circles, the benefits of counseling and support groups specializing in donor conception are invaluable. These resources provide a safe space to explore complex emotions, discuss challenges, and learn from others who have walked a similar path.
Professional counselors can offer strategies for processing grief, managing anxiety, and fostering acceptance. Support groups connect you with a community that truly understands the nuances of donor conception, offering practical advice and emotional solidarity. Engaging with these support systems can help intended parents feel less isolated and more empowered as they move forward with their family-building journey.
Discussing Donor Conception with Your Child
A critical and evolving aspect of donor conception is the decision of discussing donor conception with your child. Experts in donor-conceived individuals and family dynamics increasingly advocate for age-appropriate honesty and transparency from an early age.
This approach, often referred to as “telling and talking,” allows the child to grow up with this knowledge as an integrated part of their identity rather than discovering it as a secret later in life. Starting early, even before the child fully comprehends, normalizes the concept and makes it a natural part of family conversations.
There are numerous resources and approaches for talking to donor-conceived children about their origins, including children’s books, online communities, and professional guidance. These tools help parents frame the narrative in a positive and empowering way, emphasizing the love and intention behind their family’s creation.
Addressing potential concerns about identity and belonging is also key. Children may naturally have questions about their genetic heritage, and open dialogue helps them understand that their identity is shaped by both their genetic origins and, most importantly, by the loving family that raises them.
This proactive and honest approach fosters trust and resilience, strengthening the family unit built through donor conception.
Legal and Ethical Considerations in Donor Conception
Navigating the legal landscape surrounding donor conception is a critical step for all intended parents. The laws governing donor conception, including aspects of donor anonymity, parental rights, and disclosure, vary significantly across different countries and even within states or provinces.
What is permissible and legally binding in one region may not be in another. Some jurisdictions maintain strict donor anonymity, while others have moved towards “identity-release” or “open-identity” donation, allowing donor-conceived individuals to access identifying information about their donor upon reaching a certain age.
It is absolutely imperative to seek legal consultation for donor conception from an attorney specializing in reproductive law. This legal expert can explain the specific regulations in your area, help you understand the implications of your chosen donor type (anonymous vs. known), and ensure that all necessary legal documents are properly executed.
This includes understanding the legal parentage of the child, particularly for same-sex couples or single parents by choice, and clarifying the legal relationship between the donor and the child.
Without proper legal guidance, intended parents could face unforeseen challenges regarding parental rights or the child’s legal status in the future. A thorough understanding of these legal frameworks provides a secure foundation for your family built through donor conception.
Rights and Responsibilities of Donors and Recipients in Donor Conception
The process of donor conception involves a clear delineation of rights and responsibilities for both the donor and the recipient(s). These are typically formalized through comprehensive legal agreements. For recipients, the primary right is to become the legal parent(s) of the child conceived through the donation, with full parental authority and responsibility.
Their responsibilities include adhering to the terms of the agreement, providing a loving and stable environment for the child, and often managing the disclosure of the donor conception to the child.
For donors, their rights and responsibilities are equally defined. In anonymous donation, donors typically relinquish all parental rights and responsibilities, with no legal obligation or claim to the child. Their primary responsibility is to undergo the required medical, genetic, and psychological screening and to provide accurate information.
In known donation, the legal agreements are more intricate. They explicitly outline the donor’s lack of parental rights and responsibilities, ensuring that the intended parents are the sole legal parents. These agreements also address any potential future contact or information exchange, such as medical updates or the possibility of the donor-conceived child seeking contact later in life.
This careful legal structuring ensures clarity for all parties involved in donor conception, safeguarding the family unit and the well-being of the child.
Success Rates and What to Expect from Donor Conception
When considering donor conception, understanding the likelihood of success is a natural and important concern.
Generally, donor conception through IVF tends to have higher success rates compared to IVF cycles using a woman’s own eggs, especially if she is of advanced maternal age or has diminished ovarian reserve.
This is primarily because donor eggs typically come from younger, thoroughly screened donors with optimal fertility, leading to higher quality embryos. The success of donor egg IVF is significantly influenced by the age of the egg donor rather than the age of the recipient.
Several factors contribute to the overall success of donor conception. The recipient’s health plays a role, as does the embryo quality resulting from the fertilization of donor gametes. The clinic’s expertise and the specific protocols used by the fertility clinic also have a substantial impact on outcomes.
Reputable clinics will transparently share their donor conception success rates, often broken down by donor type (egg, sperm, embryo) and recipient age, providing realistic expectations for your fertility treatment with donor gametes. While no assisted reproductive technology guarantees a pregnancy, donor conception offers a very strong probability for many intended parents seeking to build a family.
Managing Expectations and Potential Challenges in Donor Conception
Despite generally favorable success rates, it is crucial to approach donor conception with realistic expectations. While the chances are high, success is not guaranteed in every cycle. The donor conception journey can sometimes involve multiple attempts, which can be emotionally and financially demanding. It’s important for intended parents to prepare for this possibility and cultivate emotional resilience.
Challenges might include the physical demands of medication, the emotional intensity of the two-week wait, or the disappointment of an unsuccessful cycle. Fertility clinics provide support services to help manage these aspects.
Open communication with your medical team and a strong personal support network are vital. Understanding that this path, like any in family building, can have its ups and downs allows you to better navigate the process. Focusing on long-term goals and celebrating each step forward, regardless of the immediate outcome, is key to a positive experience with donor conception.
Conclusion
The journey of donor conception through IVF with donor gametes represents a profound and often transformative path to building a family.
It is a testament to the unwavering desire to experience parenthood, offering hope and tangible solutions where traditional methods may not be viable. We’ve explored the intricate steps, from understanding the basics of donor conception and selecting a donor to navigating the medical procedures and the emotional landscape that accompanies this unique process.
Ultimately, the essence of parenthood lies not in genetic makeup but in the boundless love and nurturing provided to a child.
Families built through donor conception are as rich, diverse, and fulfilling as any other. This pathway empowers individuals and couples to realize their dreams of having children, creating strong and loving family units.
As you consider or continue your donor conception journey, remember the importance of seeking professional guidance and support. With accurate information, emotional preparedness, and a dedicated team, donor conception can lead to the incredible joy of welcoming a child into your life.
FAQ
What is donor conception?
Donor conception refers to the process of becoming pregnant and having a child using donated gametes (sperm, eggs, or embryos) from someone other than the intended parents. This includes fertility treatments like IVF with donor eggs or donor sperm.
Who typically considers donor conception?
Individuals or couples may consider donor conception for various reasons, including advanced maternal age, diminished ovarian reserve, male factor infertility, genetic conditions that could be passed on, or for same-sex couples and single individuals who wish to build a family.
Is donor conception legally recognized everywhere?
The legal landscape for donor conception varies significantly by country and even by region within countries. It’s crucial to seek legal advice to understand the specific laws regarding parental rights, donor anonymity, and disclosure in your jurisdiction before pursuing donor conception.
How do you choose a donor for donor conception?
Choosing a donor involves a comprehensive process that often includes reviewing detailed profiles, considering physical traits, medical history, educational background, and personal interests. Donors undergo rigorous medical, genetic, and psychological screening to ensure suitability for donor conception.
What are the emotional aspects of donor conception for parents?
The emotional journey of donor conception can be complex, involving feelings of grief for the loss of a genetic connection, alongside immense hope and joy. Open communication with partners, counseling, and support groups can be invaluable in navigating these emotions and embracing the realities of donor conception.