Introduction
Experiencing vaginal bleeding in the third trimester of pregnancy can be alarming, and for good reason. The third trimester spans from week 28 of pregnancy until delivery, and while some minor spotting might occur, any bleeding during this period warrants immediate medical attention.
It’s a symptom that can signal various underlying conditions, some of which are serious obstetric emergencies requiring swift intervention to protect both maternal and fetal health.
Unlike bleeding earlier in pregnancy, third trimester bleeding often indicates a more significant issue related to the placenta, cervix, or uterus. It’s estimated that between 3% and 5% of pregnancies experience some form of late pregnancy bleeding.
Understanding the potential causes and risk factors is crucial for expectant parents, but it’s equally important to remember that self-diagnosis isn’t an option. The priority should always be prompt evaluation by a healthcare professional.
This article aims to provide clear, accurate information about the common causes and risk factors associated with third trimester bleeding. We’ll delve into the specific conditions that can lead to this symptom, helping you understand why immediate medical consultation is so vital. When dealing with bleeding in the third trimester, knowledge empowers you to act decisively for a safe pregnancy outcome.
Why is Third Trimester Bleeding a Concern?
Any instance of third trimester bleeding is a significant concern for both pregnant individuals and their healthcare providers. During these final weeks of pregnancy, the stakes are high, and what might seem like a small amount of blood can sometimes indicate a rapidly evolving and potentially life-threatening situation for both the mother and the baby.

The primary worry with third trimester bleeding is the potential impact on both maternal and fetal health. Conditions causing this bleeding can lead to excessive maternal blood loss, potentially resulting in maternal mortality or the need for a blood transfusion.
For the baby, the risks include fetal distress, premature birth, or even perinatal mortality due to oxygen deprivation or other complications arising from the underlying cause of the bleeding.Furthermore, third trimester bleeding often signifies an obstetric emergency.
This isn’t a symptom to “wait and see” about. Swift diagnosis and management are critical. Depending on the cause, delays in seeking care could lead to irreversible damage or adverse outcomes.
Your healthcare team needs to quickly determine the source and severity of the late pregnancy bleeding to implement the appropriate treatment plan, which could range from close monitoring to an urgent Cesarean section or other interventions. Ignoring bleeding in the third trimester puts both lives at risk.
Placenta Previa: A Common Cause of Third Trimester Bleeding
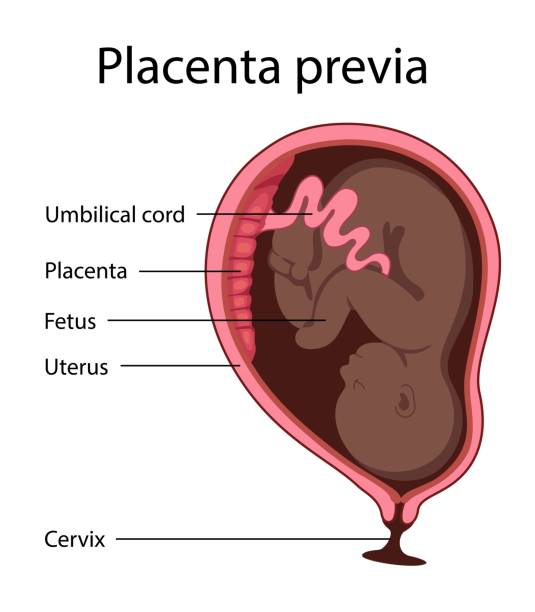
One of the most frequently encountered and significant causes of third trimester bleeding is placenta previa. This condition directly involves the placenta, the organ responsible for nourishing the fetus during pregnancy. Understanding its mechanics is key to recognizing its potential impact.
What is Placenta Previa?
Placenta previa occurs when the placenta partially or completely covers the internal cervical os, the opening of the cervix. Normally, the placenta attaches higher up in the uterus, away from the birth canal.
However, with placenta previa, its low implantation means it sits in a position that can obstruct the baby’s exit. There are different classifications: a complete placenta previa fully covers the os, a partial placenta previa covers only part of it, and a marginal placenta previa is located at the edge of the os.
Sometimes, a low-lying placenta is noted, meaning it’s in the lower uterine segment but not directly covering the os; this often resolves as the uterus grows.
Symptoms Associated with Placenta Previa
The hallmark symptom of placenta previa is characteristically painless, bright red vaginal bleeding in the third trimester. This bleeding can range from light spotting to a sudden, profuse hemorrhage. It often occurs spontaneously, without any obvious trigger, though it can sometimes be initiated by intercourse or uterine contractions.
Unlike other causes of third trimester bleeding, there is typically no associated abdominal pain or uterine tenderness. The bleeding happens because the lower uterine segment, where the placenta is attached, thins and stretches as pregnancy progresses, causing a separation between the placenta and the uterine wall and tearing blood vessels.
Risk Factors for Placenta Previa
While placenta previa can occur in any pregnancy, several factors increase an individual’s risk. A history of previous Cesarean delivery (C-section) is a major risk factor, as the scar tissue on the uterus can alter where the placenta implants.
Increasing maternal age and multiparity (having had multiple previous pregnancies) also elevate the risk. Other contributing factors include a history of previous placenta previa, smoking during pregnancy, and carrying multiple pregnancies (such as twins or triplets).
Diagnosis and Management Overview for Placenta Previa
The definitive diagnosis of placenta previa is made through an ultrasound scan. Both transabdominal and transvaginal ultrasounds can accurately pinpoint the placenta’s location. It is critically important that if third trimester bleeding is present and placenta previa is suspected or not yet ruled out, a digital cervical exam is strictly avoided.
Such an exam could inadvertently puncture the placenta or its vessels, leading to massive hemorrhage. Management typically involves close monitoring, potentially requiring hospitalization, especially if bleeding is recurrent or heavy.
Depending on the gestational age and severity, a planned Cesarean delivery is usually necessary to ensure the safety of both mother and baby, as vaginal delivery could lead to severe uncontrolled bleeding.
Placental Abruption: Another Serious Cause of Third Trimester Bleeding
While placenta previa is characterized by typically painless bleeding, another critical cause of third trimester bleeding is placental abruption, which often presents with significant discomfort. This condition involves the premature separation of the placenta from its attachment.
What is Placental Abruption?
Placental abruption occurs when the placenta detaches, either partially or completely, from the inner wall of the uterus before the baby is born. This premature separation disrupts the vital connection that delivers oxygen and nutrients to the fetus, and it can also cause significant maternal hemorrhagic shock.
The bleeding from an abruption can be either “revealed,” where blood escapes through the cervix and is visible externally, or “concealed,” where the blood collects behind the placenta within the uterus, making the external bleeding less apparent or absent despite significant internal blood loss.

Symptoms of Placental Abruption
The symptoms of placental abruption are typically more acute and painful than those of placenta previa. The classic presentation includes sudden, severe, and persistent abdominal pain, often described as a tearing or sharp sensation.
This pain is frequently accompanied by rigid or “board-like” uterine tenderness. The vaginal bleeding in the third trimester from an abruption is often dark red and may contain clots. Other signs can include back pain, rapid uterine contractions that don’t relax, and signs of fetal distress (such as changes in fetal movement or heart rate patterns).
In cases of severe concealed abruption, the mother might show signs of maternal mortality risk, such as hypotension or shock, even with minimal external bleeding.
Risk Factors for Placental Abruption
Several factors can increase the risk of placental abruption. A history of a previous placental abruption is the strongest predictor for recurrence. High blood pressure conditions, including chronic hypertension or preeclampsia, are significant risk factors.
External trauma in pregnancy, such as from a car accident or a fall, can also trigger an abruption. Lifestyle choices like cocaine use or smoking during pregnancy are strongly linked to this complication. Other risks include multiple pregnancies (e.g., twins), premature rupture of membranes, and polyhydramnios (excess amniotic fluid), which can lead to rapid changes in uterine size.
Diagnosis and Management Overview for Placental Abruption
Diagnosing placental abruption is often a clinical diagnosis, based on the presenting symptoms and physical examination findings. While an ultrasound scan can sometimes show a hematoma behind the placenta, it’s not always definitive and cannot rule out an abruption, especially in acute cases.
When third trimester bleeding is suspected to be from an abruption, immediate medical attention is paramount. Management focuses on stabilizing the mother’s condition, monitoring the fetus for fetal distress, and often, urgent delivery.
Depending on the severity of the abruption, the maternal and fetal condition, and gestational age, delivery may be via Cesarean section to expedite the process and prevent further complications. This is a critical obstetric emergency where swift action can save lives.
Other Causes of Third Trimester Bleeding
Beyond placenta previa and placental abruption, several other conditions can manifest as third trimester bleeding. While some are rarer, they can be equally, if not more, critical and demand immediate medical assessment.
Vasa Previa: A Rare but Critical Cause of Third Trimester Bleeding
Vasa previa is a particularly dangerous, though uncommon, cause of third trimester bleeding. In this condition, fetal blood vessels, often from the umbilical cord, run unprotected through the membranes and lie directly over the internal cervical os. These vessels are not cushioned by placental tissue or Wharton’s jelly, making them highly vulnerable.
The primary risk with vasa previa is that when the membranes rupture (either spontaneously or artificially), these exposed fetal vessels can tear. This leads to rapid and significant fetal blood loss, not maternal blood.
The symptoms often include painless vaginal bleeding in the third trimester that coincides precisely with the rupture of membranes. Because it’s fetal blood being lost, the baby can quickly become severely anemic, leading to acute fetal distress and potentially rapid perinatal mortality if not addressed immediately.
Diagnosis is ideally made antenatally through a specialized ultrasound scan (color Doppler). If diagnosed, a planned Cesarean delivery is almost always indicated before labor or membrane rupture to prevent this catastrophic complication.
Uterine Rupture: A Critical Obstetric Emergency
Uterine rupture is an incredibly serious, albeit rare, obstetric emergency that causes profound third trimester bleeding. It involves a full-thickness tear in the uterine wall, often at the site of a previous uterine scar, most commonly from a prior Cesarean delivery.
Symptoms can be sudden and dramatic. They include acute, severe abdominal pain that may feel like a “tearing” sensation, often followed by a sudden cessation of strong contractions. Signs of fetal distress, such as a sudden drop in fetal heart rate, are common and immediate.
The bleeding can be external vaginal bleeding in the third trimester or concealed within the abdominal cavity, leading to rapid signs of maternal mortality risk like shock.
Given its life-threatening nature for both mother and baby, uterine rupture requires immediate surgical intervention, usually an emergency Cesarean section, to deliver the baby and repair the uterus.
Less Common/Benign Causes of Third Trimester Bleeding
Not all third trimester bleeding is indicative of a severe obstetric emergency, though it should always be evaluated.
- Bloody Show: As the body prepares for labor, the cervix begins to soften, thin, and dilate. This process can dislodge the mucus plug that seals the cervix during pregnancy, leading to a small amount of pinkish or brownish mucus mixed with a few streaks of blood. This bloody show is generally light, self-limiting, and is a normal sign of impending labor, though it’s still wise to inform your provider.
- Cervical or Vaginal Lesions/Infections: Benign gynecological conditions such as cervical polyps (small growths on the cervix) or cervicitis (inflammation of the cervix) can cause light spotting in the third trimester. These conditions might bleed, especially after intercourse (post-coital bleeding) or a vaginal examination. Vaginal infections can also lead to irritation and light bleeding.
- Trauma: Direct trauma during pregnancy to the cervix or vagina, such as from intercourse or an accident, can sometimes cause minor third trimester bleeding. While often benign, the source of any bleeding needs to be confirmed by a healthcare professional.
- Undetermined Causes: In some instances, after thorough investigation, the exact cause of third trimester bleeding remains unknown. Even in these cases, vigilant monitoring is essential to ensure maternal and fetal well-being.
When to Seek Medical Attention for Third Trimester Bleeding
Given the potential seriousness of third trimester bleeding, it’s crucial to understand when and how to respond. The most important takeaway is unequivocal: any vaginal bleeding during late pregnancy demands immediate medical evaluation. Do not attempt to self-diagnose or wait to see if it resolves.
Recognizing the Urgency of Third Trimester Bleeding
Whether it’s light spotting or a heavy flow, bright red or dark, accompanied by pain or not – bleeding in the third trimester is never normal and should always be treated as a potential obstetric emergency. Delay in seeking care can have severe consequences for both the pregnant individual and the baby.
The underlying cause needs to be identified quickly to initiate appropriate treatment, which could range from close monitoring to urgent delivery. When it comes to third trimester bleeding, time is critical.
What to Do if You Experience Third Trimester Bleeding
If you experience vaginal bleeding in the third trimester, take these immediate steps:
- Contact your healthcare provider immediately or proceed directly to the nearest emergency room. Do not wait for a return call if you’re experiencing significant bleeding or other concerning symptoms.
- Note the characteristics of the bleeding: Observe the amount (e.g., how many pads are soaked), color (bright red, dark red, brown), and consistency (clots present or not).
- Note any associated symptoms: Are you experiencing abdominal pain, back pain, contractions, dizziness, faintness, or changes in fetal movement? Providing this information helps medical staff quickly assess the situation.
- Avoid intercourse, douching, or using tampons.
- Do not perform a digital vaginal examination on yourself. This is particularly important if placenta previa is a possibility, as an examination could trigger a massive hemorrhage.
Diagnostic Procedures You Can Expect for Third Trimester Bleeding
Upon arrival at a medical facility, the healthcare team will work quickly to determine the cause of your third trimester bleeding. You can expect:
- Maternal vital signs assessment: Blood pressure, heart rate, and temperature will be checked.
- Fetal heart rate monitoring: Continuous monitoring of the baby’s heart rate will assess fetal distress or well-being.
- Ultrasound: An ultrasound scan (both transabdominal and transvaginal) is a cornerstone of diagnosis. It helps determine the placenta’s location, rule out placenta previa or vasa previa, and can sometimes identify signs of placental abruption.
- Blood tests: These typically include a Complete Blood Count (CBC) to check for anemia, coagulation studies to assess clotting ability, and blood type and cross-match in case a blood transfusion is needed.
- Physical examination: After placenta previa has been ruled out by ultrasound, a speculum examination may be performed to visualize the cervix and vagina for non-placental causes of third trimester bleeding, such as cervical polyps or cervicitis. A digital cervical exam would only follow the speculum exam and after placental causes are excluded.
Your medical team will prioritize a swift and accurate diagnosis to ensure the best possible outcome for both you and your baby.
Risk Factors for Third Trimester Bleeding (Overall Summary & Prevention)
While third trimester bleeding can sometimes occur without an obvious predisposing factor, many of the serious causes are associated with identifiable risk factors.
Understanding these can help individuals and their healthcare providers manage potential risks, though it’s important to remember that having a risk factor doesn’t guarantee a complication will occur, nor does their absence guarantee a bleed won’t happen.
General Risk Factors for Third Trimester Bleeding
Across the major causes of third trimester bleeding, several common themes emerge regarding risk factors:
- Previous Uterine Surgery: A history of Cesarean delivery (C-section) is a significant risk factor for both placenta previa and uterine rupture. Any previous surgery on the uterus can alter its structure and the way the placenta implants or the integrity of the uterine wall.
- Multiparity and Advanced Maternal Age: Having had multiple previous pregnancies (multiparity) and increasing maternal age are associated with a higher likelihood of both placenta previa and placental abruption.
- Lifestyle Choices: Smoking during pregnancy and drug use, particularly cocaine, are strong and modifiable risk factors for placental abruption. These substances can impact the integrity of blood vessels and placental attachment.
- Hypertension/Preeclampsia: High blood pressure conditions, including chronic hypertension and preeclampsia, significantly increase the risk of placental abruption.
- Multiple Pregnancies: Carrying twins, triplets, or more increases the overall stress on the uterus and placenta, making third trimester bleeding more likely due to conditions like placental abruption or placenta previa.
- Previous Bleeding Episode: A history of previous placental abruption or previous placenta previa significantly elevates the risk of recurrence in subsequent pregnancies.
Minimizing Risks (Where Applicable)
While not all risk factors can be eliminated, proactive steps can help. Regular and consistent prenatal care is paramount. This allows healthcare providers to monitor for potential issues, manage pre-existing conditions like hypertension, and provide guidance on healthy lifestyle choices.
Avoiding smoking during pregnancy and drug use are direct and impactful ways to reduce the risk of certain complications leading to third trimester bleeding. Open communication with your doctor about your medical history and any new symptoms is also vital.
Importance of Early Diagnosis and Management of Third Trimester Bleeding
Ultimately, the most critical “preventive” measure for severe outcomes from third trimester bleeding is early diagnosis and swift, appropriate management.
Being aware of the signs and immediately seeking professional medical attention for any vaginal bleeding in the third trimester improves the prognosis for both the mother and the baby. Rapid assessment allows for timely interventions, from close monitoring to emergency delivery, which can be life-saving.
Conclusion
Experiencing third trimester bleeding is understandably unsettling for any expectant parent. It’s a symptom that, while sometimes benign, can indicate serious and rapidly evolving obstetric conditions that demand immediate attention.
The most critical message is clear: anyvaginal bleeding in the third trimester, regardless of how light or heavy, how painful or painless, must be evaluated by a healthcare professional without delay. Conditions such as placenta previa, placental abruption, and the rarer but life-threatening vasa previa or uterine rupture require swift and accurate diagnosis.
Prompt medical consultation for bleeding in the third trimester significantly improves the chances of positive outcomes for both the mother and the baby. By understanding the potential causes and knowing when to seek help, you are empowered to advocate for your health and your baby’s well-being during these crucial final weeks of pregnancy.
FAQ
Is light spotting in the third trimester normal?
While “bloody show”—a small amount of mucus tinged with pink or brown blood—can be normal as the cervix begins to prepare for labor, any vaginal bleeding in the third trimester should be reported to your healthcare provider immediately. Even light spotting warrants a medical evaluation to rule out serious underlying causes like placenta previa or a developing placental abruption. It’s always best to be cautious and allow a professional to assess the situation.
What does third trimester bleeding feel like if it’s serious?
The sensation accompanying serious third trimester bleeding can vary greatly. In cases of placenta previa, the bleeding is typically painless and bright red. Conversely, conditions like placental abruption often present with significant and sudden abdominal pain, back pain, and a rigid, tender uterus, along with dark, clotted bleeding. Uterine rupture would involve severe, acute pain and signs of fetal distress. It’s crucial not to rely solely on the presence or absence of pain; any bleeding itself is the red flag.
Can stress cause third trimester bleeding?
No, stress itself is not a direct cause of major obstetric complications leading to third trimester bleeding like placenta previa or placental abruption. While extreme stress can impact overall well-being during pregnancy, it does not directly trigger these specific conditions. If you experience bleeding in the third trimester, it is vital to seek prompt medical attention to identify and address a potential physical cause, rather than attributing it to stress.
How is the cause of third trimester bleeding diagnosed?
Diagnosing the cause of third trimester bleeding involves a comprehensive approach in a medical setting. Key diagnostic procedures include a thorough medical history, physical examination (often a speculum exam, but typically avoiding digital cervical exams initially if placenta previa is suspected), continuous fetal heart rate monitoring, and crucially, an ultrasound scan pregnancy. The ultrasound is essential for determining placental location and checking for other abnormalities. Blood tests, including a CBC and blood typing, are also standard.
What should I do if I experience third trimester bleeding at home?
If you experience third trimester bleeding at home, remain calm but act quickly. Immediately contact your healthcare provider or go to the nearest emergency room pregnancy. Do not insert anything into your vagina (no tampons, no douching, no intercourse). Try to note the amount, color, and any associated symptoms (pain, contractions, changes in fetal movement changes) to relay accurate information to the medical team. Do not delay seeking professional help.


