Introduction
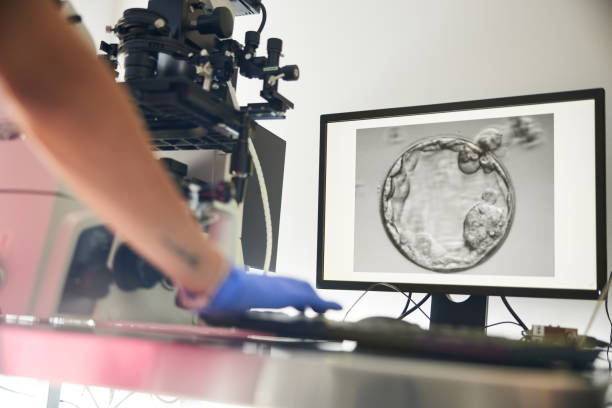
Embarking on an In Vitro Fertilization (IVF) journey often brings a mix of hope and questions. At its core, IVF is an assisted reproductive technology where an egg is fertilized by sperm in a laboratory before the resulting embryo is transferred to the uterus.
Its primary purpose is to help individuals and couples overcome various fertility challenges to achieve a successful pregnancy.
When discussing IVF outcomes, the standard metric is the live birth rate per cycle initiated. While this provides a tangible measure of the treatment’s effectiveness, it represents averages derived from large populations.
Your individual likelihood of success can vary significantly due to a multitude of factors. Understanding these contributing elements is key to setting realistic expectations and navigating your path with informed confidence.
Maternal Age: The Primary Determinant
Among the many variables influencing the outcome of fertility treatment, maternal age stands out as the single most significant factor affecting live birth rates. This strong correlation is rooted in fundamental changes in a woman’s reproductive biology.
As a woman ages, the quantity and quality of her eggs naturally decline. This decline is largely due to a reduction in ovarian reserve and an increase in chromosomal abnormalities within the remaining eggs.
- Under 35: Success rates are generally at their highest, often ranging from 40% to 50% live birth rate per cycle.
- Over 40: Rates can fall to under 10%. This steep decline occurs because older eggs are more prone to genetic errors, which can lead to embryos that either fail to implant or result in miscarriage.
The quality of eggs is paramount for successful fertilization and healthy embryo development. For women facing age-related challenges, especially those over 40, the option of using donor eggs often significantly improves their prognosis.
When donor eggs from younger women are used, the likelihood of a successful IVF pregnancy tends to reflect the age of the donor, offering a more optimistic outlook.
Female Factor Infertility and IVF Outcomes

Several conditions affecting women can influence IVF success rates:
- Blocked Fallopian Tubes: For women with blocked or damaged fallopian tubes, IVF bypasses the tubes entirely, often leading to very good IVF success rates, as the primary mechanical barrier to conception is removed.
- Endometriosis: This condition, where tissue similar to the uterine lining grows outside the uterus, can impact egg quality, implantation, and overall IVF success rates. The severity of endometriosis often dictates the prognosis; some cases may benefit from surgical intervention before IVF.
- Polycystic Ovary Syndrome (PCOS): While PCOS can cause irregular ovulation, leading to difficulty conceiving naturally, it often responds well to ovarian stimulation protocols during IVF. With careful management, women with PCOS can achieve favorable IVF success rates.
- Uterine Abnormalities: Conditions like fibroids or polyps within the uterus can interfere with embryo implantation. These are often addressed surgically prior to IVF to optimize the uterine environment and improve IVF success rates.
Male Factor Infertility and IVF Outcomes
Male infertility, ranging from low sperm count to poor motility or morphology, significantly impacts natural conception. However, IVF, particularly when combined with Intracytoplasmic Sperm Injection (ICSI), offers a robust solution.
ICSI involves injecting a single sperm directly into an egg, circumventing many male factor challenges. This technique has revolutionized treatment for male infertility, contributing to strong IVF success rates even in severe cases. Sperm quality remains vital, as healthy sperm are needed for fertilization and subsequent embryo development, directly influencing the final IVF success rates.
Unexplained Infertility: Navigating the Unknown and Its Effect on IVF Success Rates
Approximately 10-15% of couples undergoing fertility evaluation receive a diagnosis of “unexplained infertility,” meaning no specific cause can be identified.
For these couples, IVF success rates can be comparable to or slightly lower than those with identified causes, as the underlying issue, though unknown, might still affect egg, sperm, or embryo quality, or implantation. IVF often serves as a primary treatment path in these scenarios, offering a systematic way to address potential, undiagnosed problems in the fertilization or early development process.
Embryo Quality and Development
The Critical Role of Embryo Quality in Achieving IVF Pregnancy
Once fertilization occurs in the laboratory, the quality and subsequent development of the embryo become paramount factors directly impacting IVF success rates. Not all embryos are created equal, and their potential to implant and result in a healthy pregnancy varies widely.
Factors Influencing Embryo Quality
Embryo quality is assessed by embryologists based on various criteria, including the number of cells, their uniformity, and the degree of fragmentation. While the ultimate determinants are largely genetic, stemming from the quality of the egg and sperm (which, as discussed, relates heavily to age), laboratory conditions also play a crucial role.
A state-of-the-art lab environment, precise culture media, and expert embryological handling contribute significantly to healthy embryo development and consequently influence IVF success rates. Even with optimal conditions, not every fertilized egg will develop into a viable embryo suitable for transfer.
Fresh vs. Frozen Embryo Transfer: Impact on IVF Success Rates
Historically, fresh embryo transfers were the norm. However, advancements in cryopreservation techniques have popularized frozen embryo transfers (FETs). Often, FETs boast comparable, if not slightly higher, IVF success rates in many cases.
This is because a fresh transfer occurs immediately after ovarian stimulation, when a woman’s body might still be recovering from high hormone levels, which can make the uterus less receptive. With a frozen transfer, the uterus has time to return to a more natural, receptive state, allowing for a more precisely timed transfer, which can significantly enhance IVF success rates.
The ability to select the best quality embryos for freezing and transfer at an optimal time has positively impacted cumulative IVF success rates.
Preimplantation Genetic Testing (PGT): Enhancing Success and Reducing Risk
Preimplantation Genetic Testing (PGT), particularly PGT-A (aneuploidy), involves screening embryos for chromosomal abnormalities before transfer.
By identifying and selecting chromosomally normal embryos, PGT-A can reduce the risk of miscarriage and increase the likelihood of a successful implantation, thereby improving IVF success rates per embryo transferred, especially for certain patient populations, such as those with recurrent pregnancy loss or advanced maternal age.
While it doesn’t guarantee pregnancy, it optimizes the chances by ensuring only the most viable embryos are considered for transfer.
Optimizing Your Lifestyle for Enhanced IVF Success Rates
While many factors influencing IVF success rates are beyond a patient’s direct control, lifestyle choices represent an area where individuals can actively contribute to improving their chances. Adopting healthy habits can significantly impact overall reproductive health, thereby enhancing the likelihood of a successful IVF pregnancy.
Nutrition and Diet for Fertility A balanced and nutritious diet is fundamental. While no specific “fertility diet” guarantees success, evidence suggests that a Mediterranean-style diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, can positively influence fertility.
Avoiding highly processed foods, excessive sugars, and unhealthy fats is also crucial. Key nutrients like folic acid, vitamin D, and omega-3 fatty acids are particularly important for reproductive health and can indirectly support IVF success rates.
Weight and BMI: Impact on Fertility Treatment Maintaining a healthy Body Mass Index (BMI) is vital. Being either overweight or underweight can disrupt hormonal balance, affect ovulation, and reduce egg and sperm quality. For women, obesity can lead to insulin resistance and inflammation, making conception more challenging and potentially lowering IVF success rates. For men, extreme weight can negatively impact sperm parameters. Achieving a healthy weight before and during IVF can significantly improve outcomes.
Smoking and Alcohol Consumption: Detrimental Effects The negative impact of smoking and excessive alcohol consumption on fertility is well documented. Smoking, for both men and women, directly damages egg and sperm quality, reduces ovarian reserve, and can interfere with embryo implantation. Alcohol, especially in higher amounts, can also impair fertility and may reduce IVF success rates. Eliminating these habits is one of the most impactful steps a patient can take to enhance their chances.
Stress Management and Mental Well-being for IVF Success The IVF journey is inherently stressful, and while stress itself isn’t a direct cause of infertility, chronic stress can affect hormonal balance. Engaging in stress management techniques such as mindfulness, yoga, meditation, or counseling can support mental well-being throughout the process. A calm and positive mindset, though not a guarantee, can contribute to a more favorable environment for treatment and potentially aid IVF success rates.
Exercise and Physical Activity Moderate, regular exercise is beneficial for overall health and fertility. It helps maintain a healthy weight, improves blood flow, and reduces stress. However, excessive or high-intensity exercise might have a detrimental effect on some women undergoing IVF, as it can potentially alter hormonal balance. Finding a balanced exercise routine is key.
Sleep Quality: A Foundation for Reproductive Health and IVF Success Rates Adequate and quality sleep is crucial for hormonal regulation and overall bodily function. Poor sleep patterns can disrupt hormone production that is vital for reproductive health. Prioritizing 7-9 hours of restful sleep can support the body’s natural processes and potentially contribute to better IVF success rates.
The Impact of Clinic Expertise and Protocols on IVF Success Rates
While patient-specific factors are paramount, the fertility clinic itself and the specific treatment protocols employed play a substantial role in influencing IVF success rates. The expertise of the medical team, the quality of the laboratory, and the personalized nature of the treatment plan can significantly impact outcomes.

Choosing the Right Fertility Clinic for Optimal IVF Success Rates Selecting a reputable fertility clinic is a critical decision. Look for clinics with experienced doctors, highly skilled embryologists, and state-of-the-art laboratory technology. Clinic-specific IVF success rates are often reported to organizations like the Society for Assisted Reproductive Technology (SART) in the U.S. or similar national registries.
Reviewing and comparing these published IVF success rates, alongside considering factors like patient reviews and communication style, can guide your choice. A clinic that prioritizes individualized treatment plans over generic approaches is often better positioned to optimize your personal IVF success rates.
Ovarian Stimulation Protocols The protocol chosen for ovarian stimulation (to encourage egg production) is tailored to each patient’s unique profile, including age, ovarian reserve, and specific diagnosis. Different protocols, such as antagonist, agonist, or flare, aim to maximize the number of high-quality eggs retrieved while minimizing risks. The careful selection and adjustment of these protocols directly influence the quantity and quality of embryos produced, thereby affecting overall IVF success rates.
Embryo Transfer Technique for Optimal IVF Success Rates The embryo transfer procedure, though seemingly simple, is a delicate and crucial step. The skill and precision of the physician performing the transfer can significantly impact implantation rates. Factors like avoiding uterine contractions, precise placement of the embryo, and minimizing trauma to the uterine lining are all vital. A meticulous transfer technique is a significant contributor to the final IVF success rates.
Number of IVF Cycles and Cumulative Success It’s important to understand that not every IVF cycle results in a live birth. Many patients require multiple cycles to achieve a successful pregnancy. Clinics often track cumulative IVF success rates, which represent the likelihood of success over several attempts. These rates generally increase with each additional cycle, as physicians can refine protocols based on how a patient responds, continuously working to improve the chances of a positive outcome.
Additional Considerations for Your IVF Journey
Beyond the primary influences of age, infertility diagnosis, embryo quality, and clinical factors, several other elements can subtly, yet significantly, contribute to or detract from IVF success rates. These factors often receive less attention but are nonetheless important in the comprehensive picture of fertility treatment outcomes.
Previous Pregnancy History and IVF Success Rates A woman’s prior obstetric history can offer clues about her potential for future IVF success rates. A history of successful pregnancies, especially live births, can be a positive indicator, suggesting a receptive uterus and capable reproductive system. Conversely, a history of recurrent miscarriages or ectopic pregnancies might point to underlying issues that could require additional investigation or specialized management to improve IVF success rates.
Uterine Receptivity for IVF Success Rates Even with a high-quality embryo, the uterus must be receptive for successful implantation. Factors such as the thickness and quality of the uterine lining (endometrium), and the absence of conditions like chronic endometritis or immunological factors, are crucial. Assessing and optimizing uterine receptivity through various diagnostic and therapeutic interventions can play a role in boosting overall IVF success rates.
Duration of Infertility While not always a definitive predictor, the length of time a couple has been trying to conceive can sometimes correlate with IVF success rates. Longer periods of infertility might suggest more complex underlying issues that could be harder to overcome, although IVF remains a powerful tool regardless of duration.
Male Lifestyle Factors Beyond sperm parameters, the general health and lifestyle of the male partner are also relevant. Factors such as chronic health conditions, medication use, exposure to environmental toxins, and even significant stress can impact sperm quality and, consequently, influence overall IVF success rates. A holistic approach that considers both partners’ health is always recommended.
Navigating Your IVF Journey: Realistic Expectations and Support
Understanding IVF success rates is vital, but it’s equally important to approach your IVF journey with realistic expectations. IVF is a complex and highly individualized process, and while incredible strides have been made, success is never guaranteed in a single cycle. Outcomes vary widely based on the interplay of all the factors discussed, from age and diagnosis to embryo quality and clinic protocols.
Open and honest communication with your fertility specialist is paramount. They can provide a personalized assessment of your potential IVF success rates based on your unique circumstances and help you understand the most suitable treatment path.
Throughout this often emotionally challenging journey, emphasizing emotional support and mental well-being is crucial. If you are considering or embarking on IVF, consulting a fertility specialist is the essential next step for comprehensive assessment and tailored guidance toward achieving a successful IVF pregnancy.
FAQ
What is the average IVF success rate?
The average IVF success rate varies significantly by age. For women under 35, the live birth rate per cycle can be around 40-50%. These are general statistics, and your individual results will depend on many unique factors influencing IVF success rates.
Does the number of embryos transferred increase IVF success?
While transferring more embryos might seem to increase the chance of pregnancy, it also significantly raises the risk of multiple pregnancies, which carry higher health risks for both mother and babies. Most clinics now recommend single embryo transfer for optimal IVF success and safety, aiming for better overall IVF success rates without unnecessary risks.
Can lifestyle changes significantly improve my IVF success?
Yes, adopting a healthy lifestyle, including a balanced diet, maintaining a healthy weight, avoiding smoking and excessive alcohol, managing stress, and getting adequate sleep, can positively influence IVF success rates. These changes are crucial for enhancing your chances of IVF success by improving egg and sperm quality and overall reproductive health.
How many IVF cycles are typically needed for IVF success?
Many patients achieve IVF success within 2-3 cycles. Cumulative IVF success rates often increase with each additional cycle, as doctors can adjust protocols based on previous responses, thereby improving the likelihood of a successful IVF pregnancy over time.
When should I consider donor eggs/sperm for IVF success?
Donor eggs or sperm are often considered when there are significant issues with the quality or quantity of a patient’s own gametes, particularly for older women or those with specific genetic conditions. Using donor gametes can significantly improve IVF success rates in such cases.
Why do some IVF cycles fail?
IVF cycles can fail for various reasons, including poor embryo quality (often due to chromosomal abnormalities), issues with uterine receptivity, or problems during the embryo transfer process. Sometimes, despite optimal conditions, the cause of an IVF cycle failure remains unexplained, impacting the overall IVF success rates.


